What are genetic causes of male infertility?
Male infertility can in some cases be due to detrimental alterations in the man’s genetic material – his DNA. In such cases, the infertility has a genetic cause.
How common are genetic causes of male infertility?
Genetic causes can be identified in one in every four to five men with severe infertility, meaning men who have no sperm cells in the ejaculate. In cases of reduced semen quality, genetic causes are rarely found.

Which are the most common genetic causes of male infertility?
The three most common genetic causes of male infertility are Klinefelter syndrome, microdeletions of the Y chromosome, and mutation in the CTFR gene. These causes give rise to rather different situations, which are described separately below.
How are genetic causes of male fertility diagnosed?
If analysis of a semen sample shows that a man has no sperm cells or very few sperm cells in the ejaculate, the doctor will have a blood sample analysed for genetic or chromosomal alterations.
Can genetic causes of male infertility be treated?
Genetic causes of male infertility cannot be treated. However, some men who are infertile because of genetic or chromosomal alterations can still have children by use of different assisted reproduction techniques. Details are provided below for the most common genetic causes of male infertility.
Klinefelter syndrome
Klinefelter syndrome is the most common genetic cause of non-obstructive azoospermia. Non-obstructive azoospermia is the situation where no sperm is found in the ejaculate, and where this is not due to an obstruction of the ways leading the sperm from the testes to the tip of the urethra.
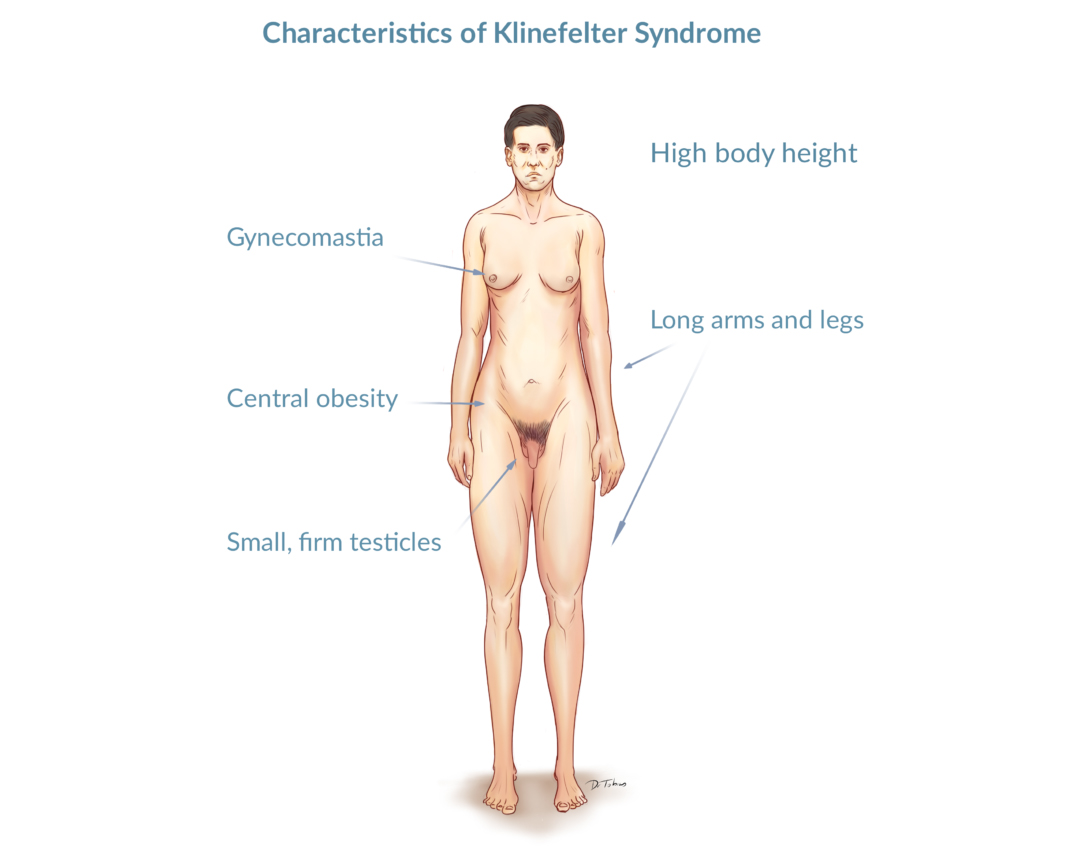
Klinefelter is a chromosomal disorder. Rather than having 46 chromosomes, including the two sex chromosomes X and Y (46,XY), boys and men with Klinefelter syndrome have an additional X chromosome (47,XXY).
Whereas most men with Klinefelter syndrome do not have any sperm in the ejaculate, mature and viable sperm can be found within the testes in about 40% of men with Klinefelter syndrome.
If a man with Klinefelter syndrome wants to genetically father a child, a procedure called testicular sperm extraction (TESE) can be used to take out sperm cells directly from the testes. Via another procedure called intracytoplasmic sperm injection (ICSI), a single sperm cell can be injected directly into an egg. The fertilized egg is transformed into a proembryo and then transferred to the female partner’s uterus.
Boys and men with Klinefelter syndrome also have a variety of other symptoms. Read more about Klinefelter syndrome here [link to text about Klinefelter syndrome]
Deletions of the Y chromosome
Sex chromosomes are called X and Y chromosomes. Whereas women have two X chromosomes, men have one X and one Y chromosome. The Y chromosome contains several genes critical for sperm production. Most of these genes are in areas of the Y chromosome called the AZF (azoospermia factor) regions. The AZF regions are constituted by the AZFa region, the AZFb region and the AZFc region.
Lack of one or more AZF regions, called AZF deletions, is a relatively common genetic cause of infertility in men with no or only few sperm cells in the ejaculate.
If a man lacks the entire AZFa region or the entire AZFb region, he is unlikely to produce any sperm cells. This is also the case, if all three AZF regions are deleted.
The most frequent type of AZF deletion is, however, a lack of the AZFc region. Men lacking the AZFc region may still produce sperm cells. This is also the case in men who has a partial deletion in one of the AZF regions.
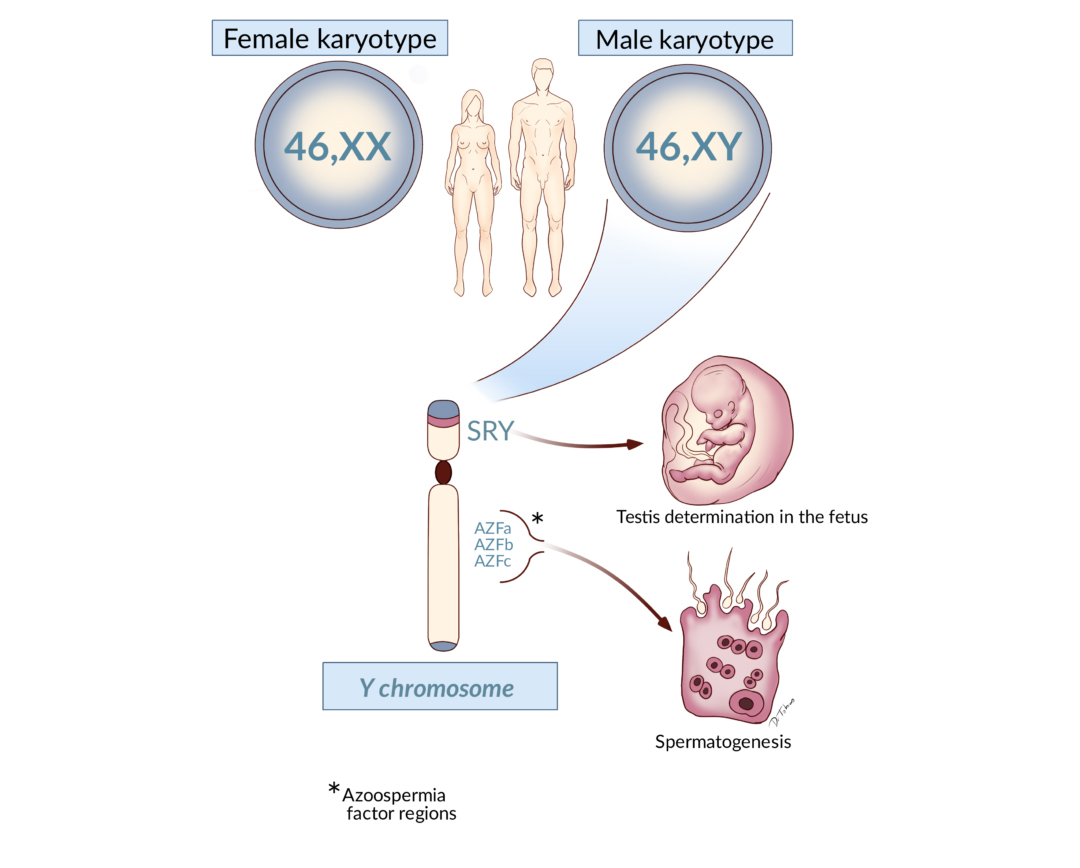
Men who have a specific partial deletion in the AZFc region, called gr/gr deletion, might have a reduced number of sperm cells in the ejaculate. However, other men with the same deletion can have normal sperm production.
Men who are infertile because of an AZF deletion might still be able to genetically father a child, if there is some degree of sperm production in his testes. Via a technique called testicular sperm extraction (TESE), viable sperm cells can be extracted directly from the testes and used for in vitro fertilization.
If a man with a Y chromosome deletion genetically fathers a son, he will inherit the Y chromosome deletion.
Mutation in the CFTR gene
The most frequent genetic form of obstructive azoospermia is caused by mutations in the CFTR gene.
Obstructive azoospermia is the situation where the transport of the sperm cells away from the testes, through the epididymis and via the vas deferens and ejaculatory ducts and the urethra is blocked, resulting in no sperm cells in the ejaculate.
Mutations in the CFTR gene cause congenital bilateral absence of the vas deferens (CBAVD). In addition, the epididymis is malformed and the seminal vesicles, which are involved in the production of seminal fluid, are absent. Consequently, the sperm cannot be transported away from the testes.
CFTR is short for cystic fibrosis transmembrane conductance regulator, and CBAVD is referred to as the genital form of cystic fibrosis. Indeed, almost all men with cystic fibrosis also have CBAVD. However, some mutations in the CFTR gene can lead to CBAVD as the only abnormality, with no other signs of cystic fibrosis.
Since sperm cells are produced in the testes, a man with obstructive azoospermia can become the genetic father of a child, if procedures are used to extract the sperm cells directly from the testes or the epididymis.
A man with mutations in the CFTR gene has the risk of getting a child that carries the CFTR gene mutations. Therefore, he and his partner should be offered genetic counselling.




















