Hypogonadotropic hypogonadism
What is male hypogonadotropic hypogonadism?
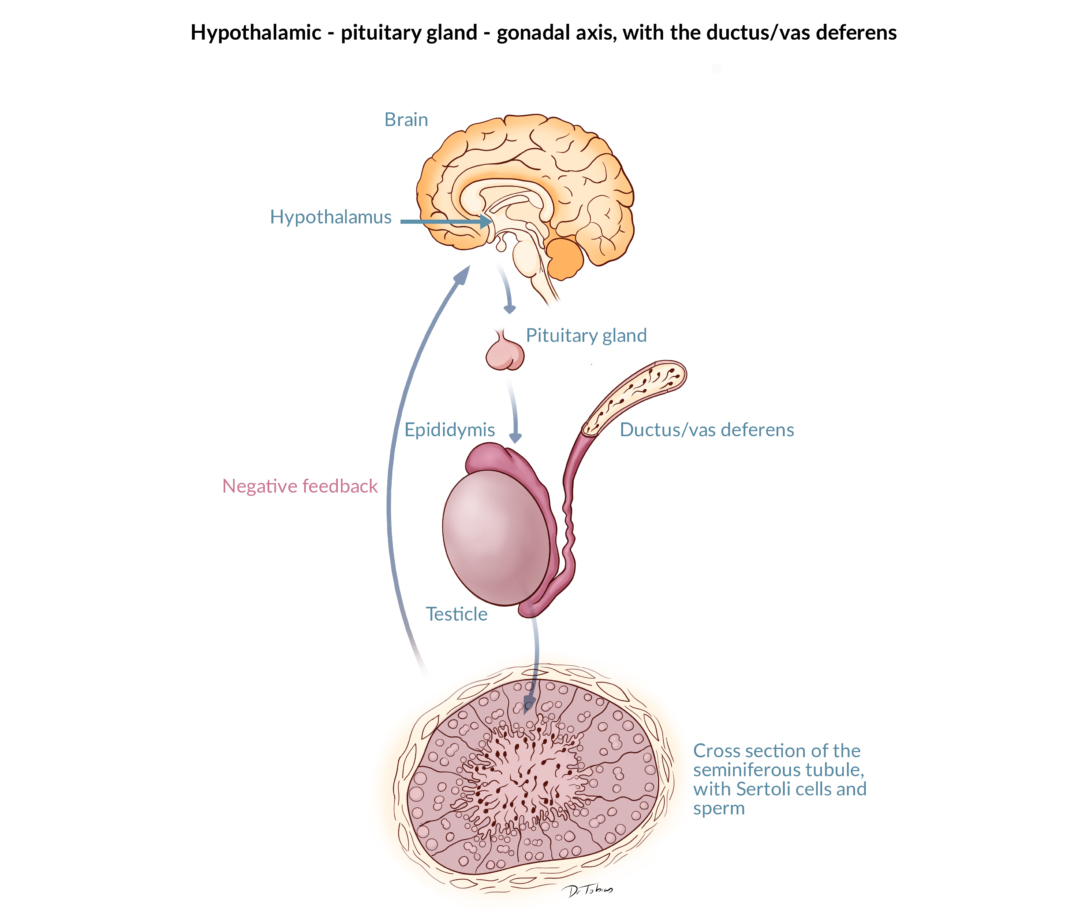
Male hypogonadism is defined as an impaired function of the testes. In male hypogonadotropic hypogonadism, the impaired testicular function is caused by insufficient hormonal stimuli from the pituitary or the hypothalamus, which are structures located in the brain.
How common is hypogonadotropic hypogonadism?
Hypogonadotropic hypogonadism can be congenital or acquired. Congenital hypogonadotropic hypogonadism is a rare condition, whereas the acquired form is relatively common.
What are the symptoms of hypogonadotropic hypogonadism?
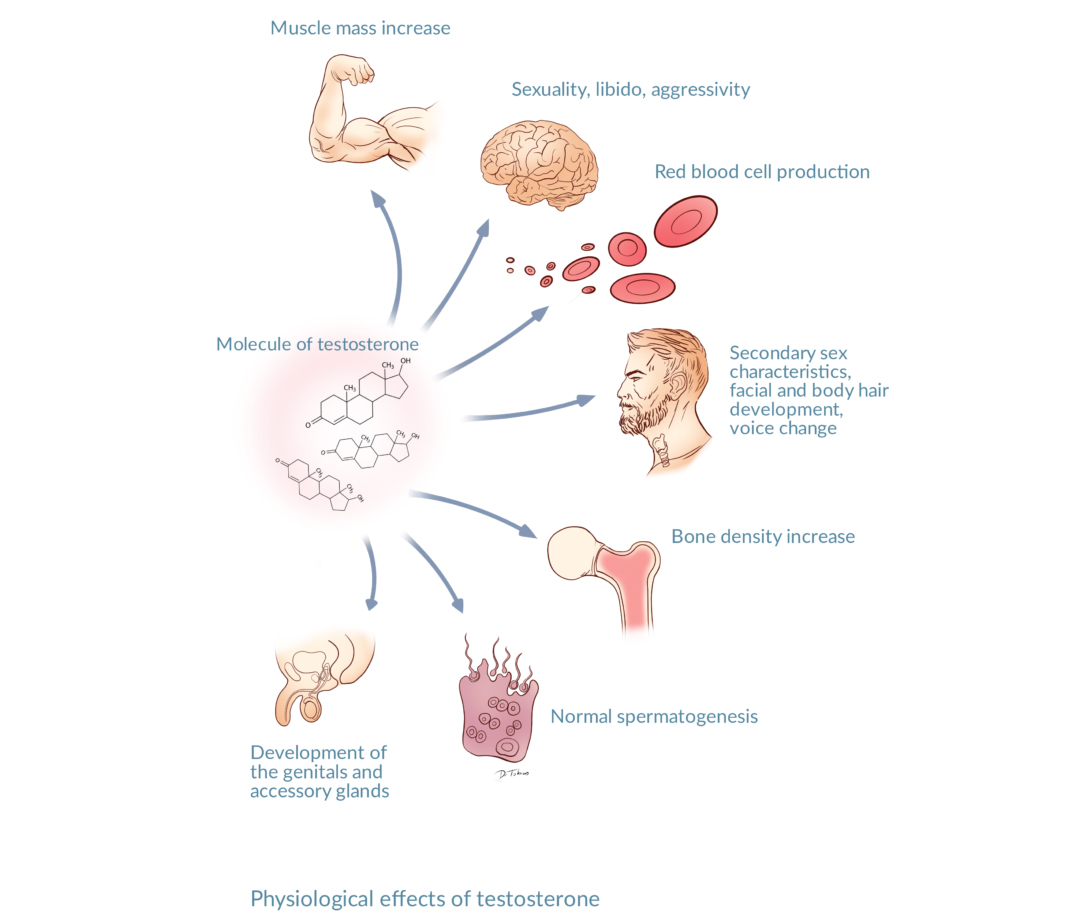
The primary functions of the testes are to produce testosterone and sperm cells. Men with a poor testicular function due to hypogonadotropic hypogonadism therefore have symptoms of androgen insufficiency and impaired spermatogenesis
Symptoms of androgen insufficiency include lack of energy, weight gain, sexual dysfunctions, and a diminished libido.
An impaired spermatogenesis means that the production of sperm cells is affected. This can cause subfertility or even infertility.
Signs of hypogonadotropic hypogonadism depend on time of onset. In adolescents, it can be difficult to distinguish the symptoms of hypogonadotropic hypogonadism from the symptoms of delayed puberty.
What are the causes of male hypogonadotropic hypogonadism?
Congenital hypogonadotropic hypogonadism normally has a genetic cause. Kallmann syndrome, caused by mutations in the KAL1 gene, is the best-defined cause of congenital hypogonadotropic hypogonadism.
Acquired hypogonadotropic hypogonadism can have multiple causes:
- Brain trauma
- Brain surgery or irradiation
- Some medications
- Abuse of anabolic steroids
- Abuse of alcohol
- Systemic diseases
While medications often lead to transient hypogonadotropic hypogonadism, it can take a long time to recover from abuse of anabolic steroids.
Who should I consult?
Diagnosis and treatment of hypogonadotropic hypogonadism should be carried out by a clinician specialized in these conditions. This will ensure the best outcome for you, both in terms of proper androgen supplementation and restoration of your fertility.
How is hypogonadotropic hypogonadism diagnosed?
You will give a blood sample, which is analysed for levels of testosterone, LH and FSH. The hormones LH and FSH, collectively known as gonadotropins, are produced in the pituitary and stimulate the testes to produce testosterone and sperm cells under normal conditions.
In case of hypogonadotropic hypogonadism, testosterone, LH and FSH levels are low.
In some cases, you will also have a GnRH stimulation test, which enables the measurement of GnRH levels. The hormone GnRH is produced in the hypothalamus and stimulates the pituitary to produce the gonadotropins LH and FSH. Measurement of GnRH helps the clinician to determine, whether the reason for insufficient gonadotropins is due to pituitary alterations or to lack of GnRH stimulation from the hypothalamus.
How is male hypogonadotropic hypogonadism treated?
Treatment with hormones acting like LH and FSH can replace the lacking pituitary hormones. In most cases, such gonadotropin replacement therapy restores sperm production and testosterone levels, and thereby alleviates or even removes the symptoms of hypogonadotropic hypogonadism.
Gonadotropin replacement therapy is, however, troublesome, requiring several injections a week. Use of portable infusion pumps administering pulses of GnRH is another option, although the price is high, and its use is restricted to highly specialized centres.
If you are an adult man, who do not have a current desire for fathering a child, treatment will focus on testosterone replacement therapy only. Testosterone therapy is available in several forms, including gels, skin patches, pills, and injections. In prepubertal boys with hypogonadotropic hypogonadism, gonadotropin replacement therapy is required to ensure a normal development of secondary sex characteristics during pubertal years. Such a treatment will be closely monitored by specialized clinicians. After puberty, gonadotropin replacement therapy can be replaced by the more convenient testosterone replacement therapy.




















